Build Back Fairer: Social Determinants, ethnicity and health
NHS Race and Health Observatory Board Member, Professor Sir Michael G. Marmot, Professor of Epidemiology, University College London
The Covid-19 pandemic exposed underlying inequalities in society and amplified them. Three striking features of the pandemic in Britain illustrate. First, is the social gradient in mortality from Covid – the greater the deprivation of area of residence, the higher the mortality rate. Second, the high Covid mortality in men and women classified as Black African, Black Caribbean, Bangladeshi, Pakistani and, to a slightly lesser extent, Indian. Third, the decline in life expectancy in the UK in 2020, put us among the countries most affected by the pandemic.
All three of these features of the nation’s health prompt our call to Build Back Fairer – the title of our Covid-19 reports. The big question is whether we, as a society and a government, can learn the lessons of the pandemic, and build back fairer.
The signs are not promising.
The fact that the social gradient in Covid mortality was predictable does not distract from its importance. In fact, the social gradient in Covid mortality looks rather similar to the social gradient in all causes. It follows that there should be two approaches to dealing with the pandemic: specific attempts to control the virus and its effects; and dealing with the social determinants of health that link to inequalities in mortality. The two are linked. Virus control measures, such as lockdown, made social and economic inequalities worse with consequent negative effects on health equity. And, of course, people in front line occupations were more exposed to the virus.
The sheer magnitude of the ethnic differences in covid mortality were a surprise. In my 2020 Review, Health Equity in England: the Marmot Review 10 Years On, we referred to health disadvantages among the ethnic groups that I listed above. We lamented the lack of routine data on mortality by ethnic group that prevented a more systematic analysis. When ONS published the evidence on the high rates of covid mortality among different ethnic groups it was truly shocking. I followed a minister on the BBC. The minister said he was concerned at these high rates and people should wash their hands. “Good advice”, I said, “and we should address structural racism”.
I came to this via the Americas. I chaired the Commission of Pan American Health Organisation (PAHO) on Equity and Health Inequalities in the Americas. We documented socioeconomic inequalities in health throughout the Americas. There were two other pervasive patterns in many countries of the Americas: high rates of health disadvantage in people of African descent and in Indigenous peoples.
My initial pass was that we had a conceptual model to explain these inequalities, one developed for the Commission on Social Determinants of Health. Inequities in power, money and resources, were structural drivers of inequities in the conditions of daily life. These, in turn, were the causes of health inequities. We labelled this approach: the causes of the causes. What was missing from this model were the effects of colonialism, of structural racism, and of lack of attention to cultural continuities. Documenting the effect of these and making recommendations to deal with them featured strongly in our report.
The English Covid mortality data showed that between half and two thirds of the excess COVID mortality in these different ethnic groups could be attributed to geography, where people live, and other socioeconomic characteristics. It suggests two approaches to understanding ethnic disadvantage in relation to covid. First, to ask why people of African, Caribbean, and South Asian origin should be more exposed to adverse socioeconomic conditions. Building on our social determinants conceptual model we could call this: the causes of the causes of the causes. A second question is what else is going on to explain the high Covid rates that is not captured by geography and socioeconomic characteristics. Here, structural racism has to be a candidate.
In my 2010 Marmot Review: Fair Society Healthy Lives, we had six domains of recommendations to reduce health inequalities:
- give every child the best start in life
- education and life-long learning
- employment and working conditions
- income adequate to lead a healthy life
- healthy and sustainable places in which to live and work
- taking a social determinants approach to prevention
In light of the above, to these we have now added a seventh recommendation:
- Tackle discrimination, racism and their outcomes.
And, for obvious reasons, an eighth:
- Pursue environmental sustainability and health equity together
The third issue is that, as a nation, we handled the pandemic badly.
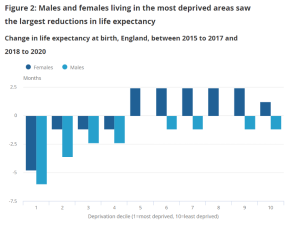
Among 20 rich countries the US had the steepest decline in life expectancy from 2019 to 2020 and 2021, followed by Scotland, Northern Ireland, Germany and England and Wales. That failure affected poorer people more. The figure shows life expectancy for the triennium 2018-20 compared to the previous three years (ONS figures). Life expectancy declined for the most deprived 40% of the population.
Arguably, the scale of impact of the Covid pandemic related to governance, the impoverished state of our public services and depth of inequalities in our society. Each of these is crucial to building back fairer.